Root Canal Treatment
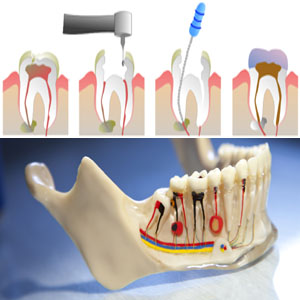
Root canal Treatment is a sequence of treatment for the pulp of a tooth which results in the elimination of infection and protection of the decontaminated tooth from future microbial invasion. This set of procedures is commonly referred to as a root canal . Root canals and their associated pulp chamber are the physical hollows within a tooth that are naturally inhabited by nerve tissue, blood vessels and other cellular entities. Endodontic therapy involves the removal of these structures, the subsequent shaping, cleaning, and decontamination of the hollows with tiny files and irrigating solutions, and the obturation (filling) of the decontaminated canals with an inert filling such as gutta percha and typically a eugenol-based cement. Epoxy resin, which may or may not contain Bisphenol A is employed to bind gutta percha in some root canal procedures.
After endodontic surgery the tooth will be “dead,” and if an infection is spread at the apex, root end surgery is required.
Although the procedure is relatively painless when done properly, the root canal remains a stereotypically fearsome dental operation.
In the situation that a tooth is considered so threatened (because of decay, cracking, etc.) that future infection is considered likely or inevitable, a pulpectomy, removal of the pulp tissue, is advisable to prevent such infection.
Usually, some inflammation and/or infection is already present within or below the tooth. To cure the infection and save the tooth, the dentist drills into the pulp chamber and removes the infected pulp and then drills the nerve out of the root canal(s) with long needle-shaped drills. After this is done, the dentist fills each of the root canals and the chamber with an inert material and seals up the opening. This procedure is known as root canal therapy. With the removal of nerves and blood supply from the tooth, it is best that the tooth be fitted with a crown.